HPR volume 13 issue 3: news (25 and 28 January)
Updated 20 December 2019
Public Health Research and Science Conference 2019, Manchester
The full programme of PHE’s annual Research and Science Conference 2019, taking place in Manchester on 9 and 10 April, has been published, covering latest developments in scientific research on protection and improvement of public health. The conference aims to strengthen scientific activity and facilitate the development of collaborations between PHE and academia. The event will celebrate the first five years operation of the NIHR’s Health Protection Research Units. More than 250 delegates attended the 2018 Warwick event, including colleagues from over 20 universities. The programme comprises five parallel streams of scientific presentations, running through both days, with plenary sessions at the beginning and end of each day, and e-poster presentation sessions each lunchtime. Late breaker paper abstracts can be submitted until the 4 February.
Venue: University of Manchester (Renold Building), Altrincham St, Manchester M1 7JA.
Conference website: www.phe-events.org.uk/phrsc19.
Five-year national AMR action plan for the UK, second WHO GLASS report
The Department of Health and Social Care has launched a new national AMR strategy to tackle antibiotic resistance within and beyond our own borders [1]. It follows the previous 2013-2018 AMR stategy that helped to reduce antibiotic use (in both humans and in food-producing animals) and to better coordinate research and strengthen surveillance in the UK. The newly published strategy is associated with two policy papers: a five-year action plan for 2019 to 2024 [2] and a long-term vision [3].
The new strategy includes international commitments to tackling the global threat of AMR through the UN General Assembly and UN Environment Programme resolutions, and G7 and G20 declarations [2]. These include the WHO’s Global Antimicrobial Resistance Surveillance System (GLASS) that the UK enrolled in in July 2017. GLASS, currently in its early implementation phase (2015-2019), aims to strengthen the evidence base on AMR through enhanced global surveillance and research, including:
- collection of information on resistance among human priority bacterial pathogens from clinical specimens (blood, urine, stool, and urethral and cervical swabs)
- collection of information on the status of participating countries’ AMR surveillance system
- provistion of guidance to countries on the development of effective AMR surveillance.
An early implementation report has been published [4] describing GLASS participation and outcomes across countries, and highlighting differences and constraints identified to date. By the end of the second data call on 31 July 2018, 69 countries were enrolled in GLASS. Forty-nine countries provided AMR data for 2017, and 67 provided a summary of their national AMR surveillance system. This included countries from all WHO regions and country economic status groups. AMR frequency in the tested population was presented by age group or infection type for five countries where population data was also reported. Compared to the first data call in 2017, GLASS has seen a 64% increase in country enrolment and more than twice the number of countries submitting AMR data in 2018.
One hundred and sixty UK laboratories participate in the GLASS scheme and the UK provided AMR data for the GLASS priority pathogens: S. pneumoniae, S. aureus, E. coli, K. pneumoniae and Acinetobacter spp isolated from blood cultures; and for E. coli and K. pneumoniae from urine specimens. The UK also updated data on the current status of the national AMR surveillance and GLASS implementation. The DHSC strategy notes that, while there was a 7.3% decrease in human antibiotic use in the UK between 2014 and 2017, drug resistant infections continue to increase; for example, the proportion of E. coli bacteraemia isolates resistant to one or more drugs increased by 23.3% in England between 2013 and 2017, indicative of increases across the UK [2].
References
- GOV.UK news story (24 January 2019). “Antimicrobial resistance: UK launches 5-year action plan and 20-year vision”.
- DHSC policy paper (24 January 2019). “UK 5-year action plan for antimicrobial resistance 2019 to 2024”.
- DHSC policy paper (24 January 2019). “UK 20-year vision for antimicrobial resistance”.
- WHO (18 January 2019). Global antimicrobial resistance surveillance system (GLASS) report: early implementation 2017-2018.
Tuberculosis in under-served populations: updated guidance
Tackling tuberculosis among under-served populations (USPs) was one of the key areas for action identified in the Collaborative TB Strategy for England, launched in 2015 [1]. This was reinforced in last year’s Annual TB Report for England which stated that, if the declines in TB rates made to date were to be maintained, preventive interventions should focus on, among other things: “addressing the social risk factors associated with TB, including the specific needs of under-served populations” [2].
PHE has updated the guidance on USPs it brought together in 2018 (comprising a number of resources including data, case studies etc) to assist those working in the field – in particular TB Control Boards, local authorities, CCGs and the third sector [3]. New information includes: updated epidemiological data; new exemplars of best practice, and links to new resources; an updated section in Chapter 7 relating to the role of local authorities; and the mapping of TB Control Board activities, included as an appendix.
For the purposes of the resource those considered to be “under-served” include: the homeless, some migrant groups, and those in contact with the criminal justice system and/or who misuse drugs or alcohol, or with mental health needs.
The resource comprises 10 chapters:
- identifying under-served populations in England and outlining the burden of TB in those populations (chapter 1, see figure)
- considering each of the main under-served populations in turn and signposting resources and exemplars of innovation and good practice (chapters 2 to 6)
- outlining the roles and responsibilities of those involved, besides TB clinical teams: ie local government, TB Control Boards, CCGs and the third sector (chapters 7, 8 and 9)
- outlining a selection of ‘models of care’ that can be used to meet the needs of USPs (chapter 10 ).
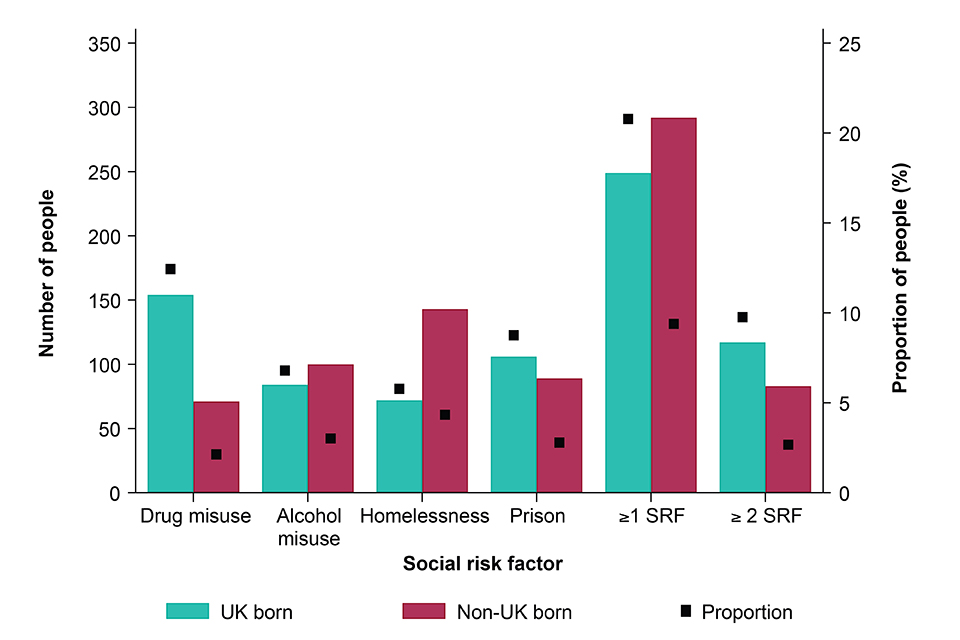
Number and proportion of people with TB (aged 15 years and above) who had social risk factors, by place of birth 2013 to 2017.
References
-
PHE (January 2015). Collaborative tuberculosis strategy for England: 2015 to 2020.
-
PHE (2018). Tuberculosis in England: 2018 report (presenting data to end of 2017).
-
PHE website (January 2019). Tackling TB in under-served populations: a resource for TB Control Boards and their partners (January 2019).
Infection and vacccine coverage reports in this issue of HPR
Infection reports
Laboratory reports of hepatitis A and C in England and Wales: July to September 2018
Vaccine coverage reports
Meningococcal ACWY school-based programme: vaccine coverage estimates, England, to 31 August 2018.
Td/IPV school-based programme: vaccine coverage estimates, England, to 31 August 2018.
