HPR volume 13 issue 11: news (29 March)
Updated 20 December 2019
Group A streptococcal infections: second report on seasonal activity in summary
Public Health England (PHE) continues to monitor notifications of scarlet fever cases in England, following the high levels recorded last spring.
According to the second report on Group A Streptococcus activity for the 2018 to 2019 season [1], typical scarlet fever increases are being reported across England.
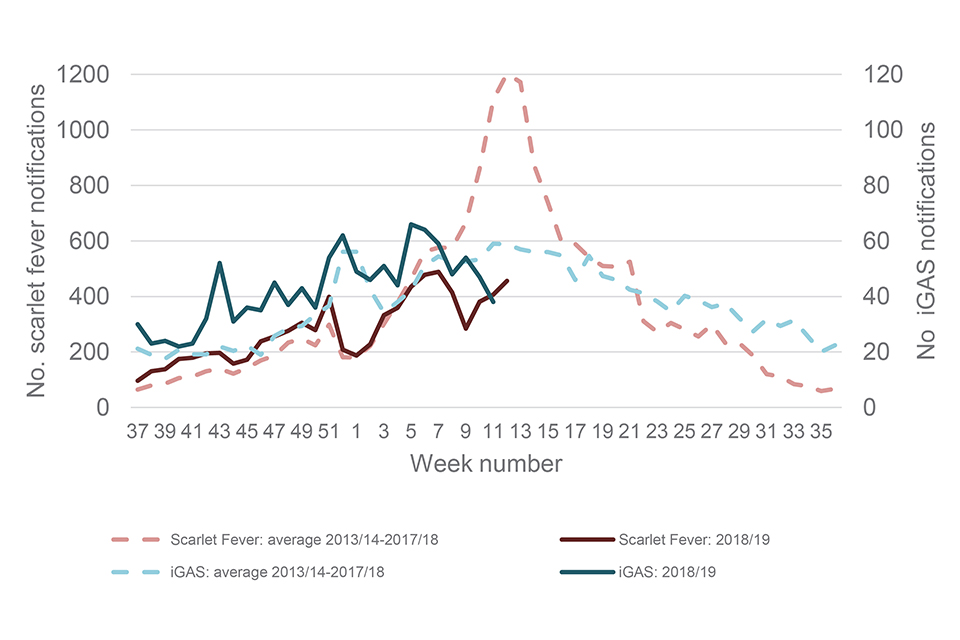
The graph below compares the latest surveillance data for both scarlet fever and invasive group A streptococcal infection (iGAS) with comparable data from previous seasons. As of 27 March 2019, scarlet fever activity is lower than seen at this time point in the last few seasons, and iGAS rates above average, but within the upper bounds of normal seasonal levels for this time of year.
In the current season to week 12 of 2019:
- a total of 7,854 scarlet fever notifications had been made, with 456 notifications made in week 12
- a total of 1,151 iGAS disease notifications had been reported through laboratory surveillance
Weekly scarlet fever and iGAS notifications in England, 2010/11 onwards
GPs, microbiologists and paediatricians are reminded of the importance of prompt notification of scarlet fever cases and outbreaks to local PHE health protection teams, obtaining throat swabs (prior to commencing antibiotics) when there is uncertainty about the diagnosis, and ensuring exclusion from school or work, until antibiotic treatment has been received for 24 hours [2]. Due to rare but potentially severe complications associated with GAS infections, clinicians and HPTs should continue to be mindful of the recent increases in invasive disease and maintain a high degree of clinical suspicion when assessing patients.
The full report includes information from M protein gene (emm) strain diversity testing and antimicrobial susceptibility data [1].
References
- Group A streptococcal infections: second report on seasonal activity, 2018 to 2019.
- PHE (2017). Interim guidelines for the public health management of scarlet fever outbreaks in schools, nurseries and other childcare settings.
Mandatory HCAI reports quarterly trends: October to December 2018
PHE’s latest quarterly epidemiological commentary on trends in reports of Staphylococcus aureus (MRSA and MSSA) and Gram-negative bacteraemia, and of Clostridium difficile infections, mandatorily reported by NHS acute trusts in England up to October to December 2018, has been published on GOV.UK [1].
Some relevant facts are listed below.
MRSA bacteraemia
There was a steep decline of 85% in the incidence rate of all reported MRSA cases between April to June 2007 and January to March 2014 – from 10.2 to 1.5 per 100,000 population. The rate remained broadly stable – at around 1.5 to 1.7 cases per 100,000 population – between January to March 2014 and October to December 2018.
MSSA bacteraemia
All reported cases of MSSA bacteraemia increased by 39% – from 2,191 to 3,057 – between January to March 2011 and October to December 2018. This was accompanied by a 30% increase in incidence rate – from 16.8 to 21.8 per 100,000 population.
The count and incidence rate of community-onset cases increased by 51% and 41%, respectively – from 1,464 to 2,172 cases, and from 11.2 to 15.8 cases per 100,000 population. Over the same period, both the count and incidence rate of hospital-onset cases increased by 14% (735 to 840 cases) and 15% (8.4 to 9.6 cases per 100,000 bed-days), respectively.
Escherichia coli bacteraemia
Between July to September 2011 and October to December 2018, both the count and incidence rate of all reported cases of E. coli bacteraemia increased by 28% – from 8,725 to 10,612 cases and from 61.8 to 75.7 cases per 100,000 population.
Similarly, over the same period, both the count and incidence rate of community-onset cases increased by 39% – from 6,279 to 8,741 cases, and from 46.9 to 62.4 cases per 100,000 population. The incidence rate of hospital-onset cases decreased 9% from 23.7 (total recorded cases: 1,996) to 21.4 (total recorded cases: 1,871) per 100,000 bed-days.
Klebsiella spp. bacteraemia
Between April to June 2017 and October to December 2018, there was a 15% increase in the count and a 13% increase in the incidence rate of all reported Klebsiella spp. bacteraemia – from 2,339 to 2,680 cases and from 16.9 to 19.1 cases per 100,000 population, respectively.
The count and the incidence rate of community-onset cases increased by 12% and 11% respectively – from 1,674 to 1,882 cases and from 12.1 to 13.4 cases per 100,000 population. Over the same period, the count of hospital-onset cases increased by 20% – from 665 to 798 cases – and the incidence rate by 18% – from 7.7 to 9.1 cases per 100,000 bed-days.
Pseudomonas aeruginosa bacteraemia
Between and April to June 2017 and October to December 2018, there was a 5% increase in the count of P. aeruginosa infections from 1,011 to 1,066 cases - accordingly, the incidence rate also increased during this period by 4% from 7.3 to 7.6 cases per 100,000 population.
Over the same period the count and incidence rate of community-onset cases increased 7% and 6%, respectively – from 637 to 680 cases and from 4.6 to 4.9 cases per 100,000 population. The count and incidence rate of hospital-onset cases remained broadly similar at 374 to 386 cases and 4.3 to 4.4 reports per 100,000 bed-days over the period.
Clostridium difficile infection
Most of the decrease in the incidence rate of CDI occurred between April to June 2007 and January to March 2012 with a 78% decrease in all reported cases – from 16,864 to 3,711 cases – and an associated 79% reduction in incidence rate, from 131.6 to 27.9. Subsequently, between January to March 2012 and October to December 2018, the count of all reported cases fell by 24% – from 3,711 to 2,827 cases – and the incidence rate reduced by 28% from 27.9 and 20.2.
There were similar, but greater, reductions among hospital-onset CDI cases: an 85% reduction in cases – from 10,436 to 1,613 – and an 84% reduction in the incidence rate, from 112.5 to 18.2 per 100,000 bed-days between April to June 2007 and January to March 2012.
This was followed by a further 42% decrease in cases – from 1,613 to 938 – and a decrease of 41% in the incidence rate, from 18.2 to 10.8 cases per 100,000 bed-days between January to March 2012 and October to December 2018.
Reference
- PHE (14 March 2019). Quarterly epidemiological commentary: mandatory MRSA, MSSA, Gram-negative bacteraemia, and C. difficile infection data (up to October to December 2018).
Infection and vaccine coverage reports in this issue of HPR
-
Group A streptococcal infections: second report on seasonal activity, 2018 to 2019
