HPR volume 12 issue 43: news (30 November)
Updated 21 December 2018
Progress towards ending the HIV epidemic in the UK
Public Health England (PHE) has published Progress Towards Ending the HIV Epidemic in the UK: 2018 Report, which provides analysis and public health interpretation of the latest epidemiological data [1]. This article summarises key findings and implications from the report.
Total number living with HIV estimated at more than 100,000
In 2017, an estimated 101,600 (95% credible interval (CrI) 99,300 to 106,400) people were living with HIV infection in the UK and 8% of this population were unaware of their infection. There were an estimated 4,200 (CrI 2,300 to 8,700) gay and bisexual men and 3,200 (CrI 2,500 to 4,900) heterosexual men and women among those living with an undiagnosed HIV infection.
UNAIDS targets met in the UK
For the first time, the UNAIDS 90:90:90 targets [2] have been met in the UK. An estimated 92% of people living with HIV in the UK were diagnosed, 98% were on treatment, and 97% of those on treatment were virally suppressed. Overall, 87% of people living with HIV in the UK have an undetectable viral load and are unable to pass on their infection.
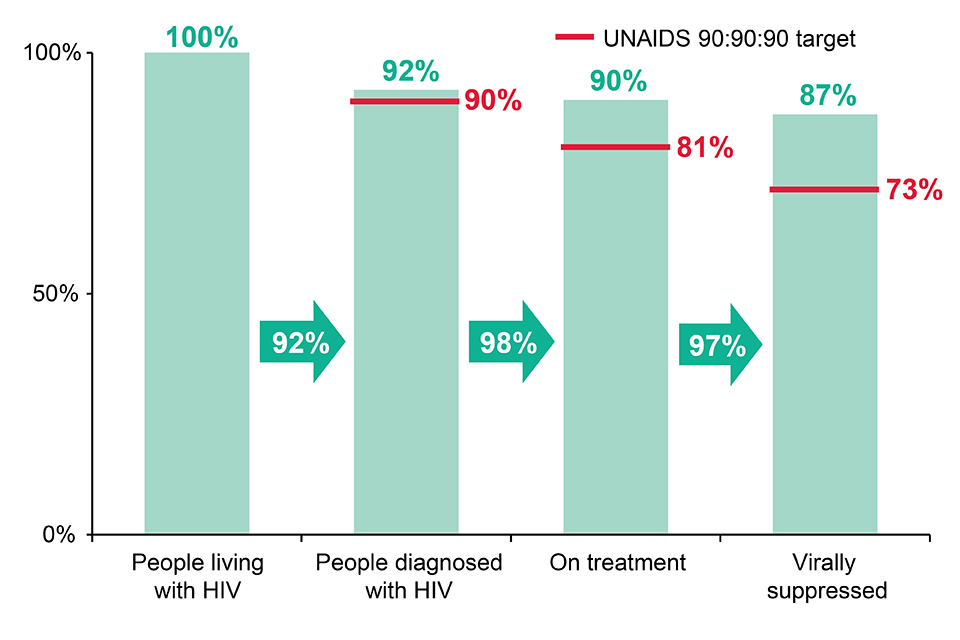
Continuum of HIV care, UK: 2017
Continued decline in transmission among gay and bisexual men
The estimated annual number of new infections acquired by gay and bisexual men has more than halved from a peak of around 2,700 (CrI 2,200 to 3,200) in 2012 to 1,200 (CrI 600 to 2,100) in 2017. The decline in new HIV diagnoses has also continued (31%, from 3,390 in 2015 to 2,330 in 2017).
The reduction in transmission shows that combination HIV prevention is working. Current key components of combination HIV prevention in the UK include condom provision, pre-exposure prophylaxis (PrEP), expanded HIV testing and prompt initiation of treatment after diagnosis (treatment as prevention). HIV testing, including repeat testing among gay and bisexual men, has led to reductions in the number living with undiagnosed infection.
The number of gay and bisexual men tested for HIV in sexual health services increased by 46% between 2013 and 2017, from 79,598 to 116,071. In 2017, 42% (45,804/108,548) of gay and bisexual men testing for HIV at a specialist sexual health service had at least one HIV test at the same service before during the previous year. In addition to increased testing, it was estimated 3,000 gay and bisexual men were taking PrEP by the end of 2016 and with the start of the PrEP Impact Trial in England, as well as PrEP programmes and studies in Scotland and Wales, this number will have increased again during 2017. Finally, initiation of treatment within 91 days of diagnosis has increased from 30% in 2013 to 77% in 2017, which reflects changes in national treatment guidelines.
Decline in heterosexuals
Declines have been observed for the first time among non-black African and non-black Caribbean heterosexual men. The largest fall was among white heterosexual men (31%, 429 to 296), men born in the UK (33%, 354 to 237) and men aged 65 years and above (55%, 47 to 21) and 15 to 34 years (32%, 148 to 101).
Clinical outcomes poorer among people who inject drugs (PWID)
Overall, HIV clinical outcomes are high across all groups. However, a significant proportion (47%) of people who inject drugs (PWID) were diagnosed at a late stage of HIV infection (CD4 cell count <350 cells per cubic millimetre within 91 days of HIV diagnosis) and even among those diagnosed promptly (CD4 count ≥350 cpcm), only 59% started treatment within 91 days of diagnosis compared to 75% overall. Retention in HIV care was also lower among PWID; 7% had not received HIV care since 2015 compared to 3% overall.
Health-related quality of life among people living with diagnosed HIV
Supporting people with HIV to maintain a good health-related quality of life is increasingly important to safeguard good clinical HIV outcomes into the future. Significantly lower health-related quality of life scores was reported by people living with HIV (0.60, on a scale of 0 to 1 where 0 is the worst possible health and 1 the best) compared to the general English population (0.86). This disparity was largely driven by poor mental health, with half of people with HIV having symptoms of depression and anxiety, compared to 24% of the general public.
Number of late diagnoses declining
The number of HIV diagnoses made at a late stage of infection decreased from 3,895 in 2008 to 1,879 in 2017. Despite this decline, the proportion of late diagnoses remains high, particularly in black African heterosexual men and women (69% and 52%, respectively) and those aged 50 to 64 years and over 65 years (55% and 61%, respectively) in 2017.
In order to reduce late HIV diagnoses, NICE quality standards focus on the expansion of HIV testing in general practice and hospitals, and testing in the presence of HIV indicator conditions. In 2017, HIV test positivity was higher in A&E (0.7%) and other secondary care settings (0.6%) than in sexual health services (SHS) (0.1%). In general practice, HIV testing rates in extremely high prevalence areas (140/10,000) were greater than in high prevalence areas (80/10,000), and over four times greater than in low prevalence areas (35/10,000).
Missed opportunities for HIV testing
Testing activity at SHS has continued to increase in 2017 and despite over 1.1 million people being tested for HIV in 2017, there are still many missed opportunities for testing in SHS. Nearly 350,000 SHS attendees were not offered a test for HIV in 2017, despite being recorded as eligible for testing. This includes over 10,000 gay and bisexual men and over 10,000 black African heterosexual men and women. However, only one third of PWID who had accessed a clinical service in the previous year had been tested for HIV.
HIV partner notification has one of the highest positivity rates of all HIV testing activities (4.3%). However, the number of people known to have tested at an SHS as a result of partner notification remains low (1,603).
References
- PHE (29 November 2018). Progress towards ending the HIV epidemic in the UK: 2018 report
- UNAIDS (2014). 90-90-90: an ambitious treatment target to help end the AIDS epidemic.
HCV treatment monitoring report and patient re-engagement exercise
PHE and NHS England have launched a national patient re-engagement exercise to identify and treat patients who have been diagnosed with hepatitis C in the past but who may have not previously had access to the most up-to-date and effective treatments [1].
The launch of the exercise coincides with the publication of the first report on data from a recently established NHS England hepatitis C patient registry and treatment monitoring system [2].
Recent improvements in hepatitis C treatment mean that therapies can now be more easily and safely rolled out into communities and outreach settings where more of the infected population can access them. Data in the treatment monitoring report indicate that 95% of those who received and completed hepatitis C treatment in the last 3 years have been cured.
Establishment of the first national patient registry and treatment monitoring system – and investment of several million pounds in treatments by NHSE [1] – represents a significant step towards the attainment of the WHO’s Global Health Sector Strategy goals for the elimination of viral hepatitis as a major public health threat by 2030 [2,3]. The WHO target is for 90% of those infected to have been diagnosed, and 80% of those diagnosed to have been treated by that date.
People who inject drugs are the largest group at risk of acquiring hepatitis C infection (the likely infection route for 70% of those currently under treatment). But the re-engagement exercise is also targeting individuals with other putative risk factors (for example those who acquired their infections abroad in countries with a high prevalence of HCV infection, or via transfusion or receipt of blood products in the UK prior to the introduction of HCV screening). It is estimated that tens of thousands of people who have been previously diagnosed with HCV are not currently on the patient register and not currently in contact with treatment services.
References
- ‘PHE and NHSE launch national drive to trace hepatitis C patients’, PHE website news story, 21 November 2018.
- PHE (21 November 2018). Hepatitis C treatment monitoring in England report (data to end April 2018).
- WHO (June 2016). Global health sector strategy on viral hepatitis 2016-2021: Towards ending viral hepatitis.
Urinary tract infections: quick reference guide for primary care
Urinary tract infections (UTIs) are common, affecting 11% of women annually and are a leading risk factor for gram-negative bloodstream infections (BSIs) [1]. Therefore optimising diagnosis and management is vital in order to reduce morbidity, BSIs, sepsis and help control antimicrobial resistance.
PHE has worked with multiple stakeholders to review and improve the PHE UTI diagnostic quick reference tools. This has included an extensive literature review and a needs assessment that explored GP surgery and care home staff management of UTIs. Members of the public were interviewed about their concerns and expectations specific to the management and prevention of suspected UTI, and stakeholder workshops were held to discuss findings and resource development.
Key findings and resulting updates were as follows:
- management of suspected UTI in younger and older patients should be different and therefore separate flowcharts were produced for different age groups including women under 65 years, adults over 65 years and children under 16 years
- in over-65-year-old patients with suspected UTI many staff in all settings incorrectly relied on urine dipstick result to inform management. The new over-65-year-old flowchart makes it very clear that dipsticks should not be used in this age group and that asymptomatic bacteriuria should not be treated in most cases
- as resistance is increasing the flowcharts encourage safety netting advice using the TARGET UTI leaflets. And urine culture in ALL OLDER patients in whom antibiotics are advised, or in those with an increased risk of antibiotic resistance
- there are now some large UK based studies of the diagnosis of UTI in younger patients, which indicate that three criteria help to discriminate those with proven UTI: dysuria, new nocturia and cloudy urine. Therefore the flowcharts and UTI leaflet for women under 65 years have been updated to reflect this new evidence
- the importance of considering sepsis and pyelonephritis was not previously highlighted in the PHE UTI diagnostic flowcharts and both of these issues were considered important by staff and patients in the needs assessment. In the new flowcharts, these are flagged in the diagnostic processes. Key resources to help in the diagnosis of sepsis are explained more extensively in the flowchart rationale (NICE, NEWS2, and RCGP)
- patients welcomed the development of a UTI leaflet for older adults. The TARGET treating your infection (TYI) UTI leaflets for women under 65 and older adults can be used to communicate key messages around prevention of UTI, typical sign or symptoms, management of UTI and safety netting for adults with suspected UTI
The newly updated diagnostic flowcharts and leaflet for older adults carry NICE endorsement that they align with treatment options recommended in the newly launched NICE and PHE guidelines on antimicrobial prescribing for recurrent, lower and upper UTI and prostatitis.
Reference
- Butler CC, Hawking MK, Quigley A, McNulty CA (2015). Incidence, severity, help seeking, and management of uncomplicated urinary tract infection: a population-based survey. Br J Gen Pract. 65(639): e702 to 707.
SMI on screening and monitoring for hepatitis E infection
First documented in 1955, hepatitis E virus (HEV) is increasingly common in the UK with an excess of 100,000 infections estimated to occur annually in England, of which a minority, less than 1%, are associated with clinically apparent disease. Although HEV often causes an acute and self-limiting infection, it has the potential of developing into a chronic infection in immunosuppressed hosts.
The clinical presentation of acute symptomatic hepatitis E infection cannot be distinguished from that of any other viral hepatitis. Although epidemiological features may suggest HEV infection in some cases, laboratory tests should always be performed to confirm any clinical diagnosis.
UK Standards for Microbiology Investigations (UK SMI) has issued a new virology standard, Screening and Monitoring for Hepatitis E Infection [1], to serve as a diagnostic tool covering the screening of blood, plasma and serum samples for HEV, using HEV antibody enzyme immunoassay (EIA) screening. It also covers the use of Nucleic Acid Amplification Tests (NAAT) for the detection of HEV RNA in plasma, serum and faeces samples for confirmation of HEV serology results, screening in the immunocompromised patient and monitoring of the treatment response.
The new UK SMI document recognises the clinical importance of HEV infection and includes comprehensive algorithms and detailed reporting tables to help laboratories screen, monitor, interpret and report laboratory findings. It is important to consider hepatitis E as a potential cause of viral hepatitis early on in the assessment of the patient, ie as part of an initial acute viral hepatitis screen and as a cause of transaminitis in the immunosuppressed hosts.
Updates on newly issued and amended standards, consultations and other developments relating to UK SMI documents are available on subscription via the Subscriber Preferences Page.
Reference
- PHE (November 2018). Screening and monitoring for hepatitis E infection (V53).
