HPR volume 11 issue 3: news (20 January)
Updated 15 December 2017
1. NaTHNaC reminds travellers to think about yellow fever vaccination before travelling to Brazil
On 18 January 2017, the National Travel Health Network and Centre published an update about the yellow fever outbreak in the state of Minas Gerais, south-eastern Brazil [1].
As of 19 January 2017, a total of 206 suspected cases including 54 deaths had been reported in Minas Gerais since 18 December 2016; 34 cases have been confirmed of which 23 cases have been fatal [2]. In addition, as of 19 January 2017, eight suspected cases have been reported in the neighbouring state of Espírito Santo, a region previously considered to be no risk for YF transmission.
Yellow fever is endemic in parts of Brazil, with occasional jungle (or sylvatic) outbreaks reported. NaTHNaC reminds travellers who are travelling to or through areas of Brazil, or any other countries with risk of YF, that vaccination is recommended for personal protection; also mosquito bite avoidance measures.
An individual risk assessment should be conducted for all travellers to areas of Brazil currently experiencing a YF outbreak, including Espírito Santo; further information is available on the NaTHNaC Country Information Page for Brazil. Health professionals should contact the NaTHNaC advice line for further guidance.
General information about yellow fever is also available on the PHE website.
1.1 References
- NaTHNaC (18 January). Yellow Fever outbreak in Brazil.
- Brazil Ministry of Health (19 January).
2. Latest flu report shows good vaccine uptake in HCWs
Public Health England surveillance systems continue to indicate widespread influenza circulation during the week-ending 15 January with some indicators increasing (GP consultations for influenza-like illness and influenza-related hospital admissions) while others remain at similar level to the previous week (influenza-associated outbreaks in the community, the proportion of laboratory confirmed influenza samples and influenza-related admissions to intensive care). Further details are provided in the latest weekly national influenza report published by PHE on 19 January [1].
The latest influenza vaccine uptake figures, as at week-ending 15 January, show that, of the 90.9% of GP practices submitting data to PHE, the estimated proportion of the population who received the 2016/17 influenza vaccine by target group was: 47.9% in under 65 years in a clinical risk group, 44.5% in pregnant women and 70.2% in 65+ year olds. The provisional, estimated proportion of children in England who received the 2016/17 influenza vaccine up to week ending 15 January was: 38.5% in all two-year olds, 40.9% in all three-year olds and 33.3% in all four-year olds.
Up to 31 December 2016, there had been a significant increase in vaccine uptake among front-line healthcare workers, compared to the same period last season: 61.9%, for the third monthly collection of uptake data, compared to 47.6% vaccinated in the same period in 2015/16. A detailed report on uptake among HCWs at Trust level is available [2].
2.1 References
- PHE (19 January). PHE Weekly National Influenza Report. See Weekly national flu reports.
- PHE (19 January). Seasonal flu vaccine uptake in healthcare workers: 1 September 2016 to 31 December 2016.
3. New resource addresses needs of under-served populations susceptible to TB
Tackling tuberculosis among under-served populations (USPs) was one of the key areas for action identified in the Collaborative TB Strategy for England in 2015 [1]. This was re-inforced in last year’s Annual TB Report for England which stated that, if the declines in TB rates made to date were to be maintained, preventive interventions should focus on a number of areas, including: “addressing the social risk factors associated with TB, including the specific needs of under-served populations” [2].
PHE has now brought together in a single document a number of resources (data, guidance, case studies etc) to assist those working in the field, either singly or in multi-agency programmes – in particular TB Control Boards, local authorities, CCGs and the third sector – to tackle the needs of the under-served [3].
For the purpose of the resource those considered to be “under-served” include: people who are homeless; some migrants groups; people in contact with the criminal justice system; people who misuse drugs and/or alcohol; and those with mental health needs.
The new resource comprises 10 chapters:
- chapter 1 defines who under-served populations are, outlines the burden of TB in these populations and maps where they are found in England
- chapters 2 to 6 take each of the main under-served populations in turn and defines them; outlines the burden of TB within these groups (see figure); discusses the challenges to be overcome; and then makes recommendations on how to meet these challenges.
- chapters 7, 8 and 9 outline the roles and responsibilities of those involved alongside the TB clinical teams (local government, TB Control Boards, CCGs and the third sector) in meeting the needs of under-served populations
- chapter 10 outlines a selection of ‘models of care’ that can be used to meet the needs of under-served populations with TB.
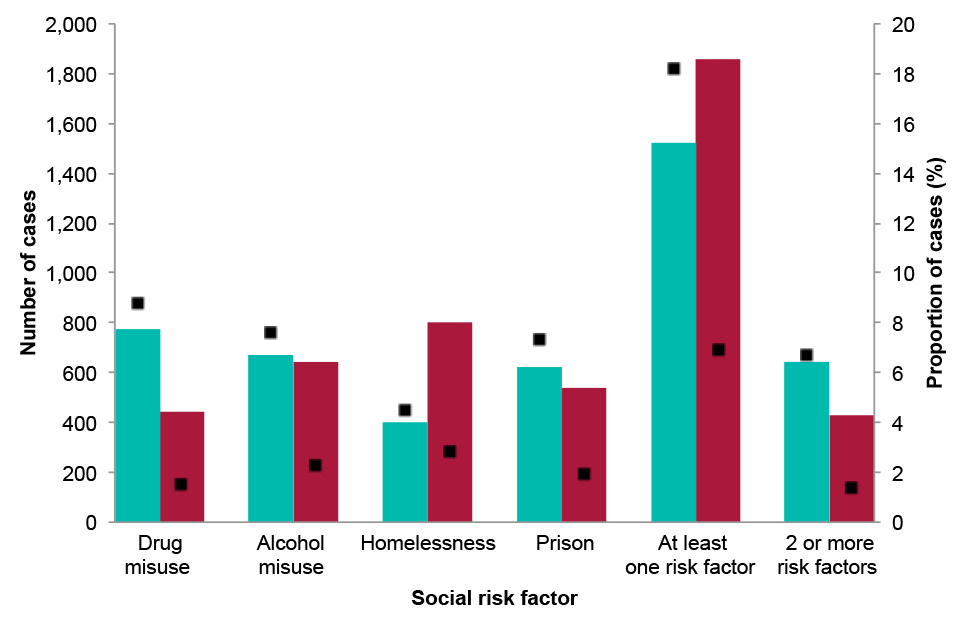
Number and proportion of TB cases (>15 years) with social risk factors, by place of birth, 2010-2015 (UK-born: cyan; non-UK born: red; proportion of cases: black)
PHE is encouraging TB Control Boards and their partners to develop services that better meet the needs of under-served groups susceptible to TB and thus mitigate the health inequalities commonly associated with TB. Chapters 2 to 6 of the new document includes hyperlinked resources and exemplars of innovation and good practice to stimulate local action.
3.1 References
-
PHE (January 2015). Collaborative tuberculosis strategy for England: 2015 to 2020.
-
PHE (2016). Tuberculosis in England: 2016 report (presenting data to end of 2015).
-
PHE website (January 2017). Tackling TB in under-served populations: a resource for TB Control Boards and their partners.
4. Updated advice on contact with animals during pregnancy
Advice which should be given to pregnant women about infections transmissible via contact with animals, particularly those giving birth, has been updated on the PHE website [1].
In order to protect their own health and that of their unborn child, women who are, or who may be, pregnant should be advised to avoid close contact with livestock animals. This is because infectious organisms may be present in birth fluids of animals, particularly sheep, cattle and goats. Such organisms may result in infections such as chlamydiosis, listeriosis, Q fever and toxoplasmosis. Different animal species are involved which give birth at different times of the year, meaning that the risks are not only confined to the spring when the majority of lambs are born. Although these infections are uncommon, and the number of human pregnancies affected by contact with sheep is extremely small, it is important that pregnant women are made aware of the potential risks in order to safeguard their health and that of their unborn baby.
The updated advice states that pregnant women should:
- not help ewes to lamb, or provide assistance to a cow that is calving or a nanny goat that is kidding
- avoid contact with aborted or new-born lambs, calves or kids or with the afterbirth, birthing fluids or materials such as bedding contaminated by such birth products
- avoid handling or washing clothing, boots or any materials that may have come into contact with animals that have recently given birth, their young or afterbirths, potentially contaminated clothing will be safe to handle after being washed on a hot cycle
- ensure that contacts or partners who have attended animals giving birth take appropriate health and hygiene precautions. This includes wearing personal protective equipment and clothing and adequate washing to remove any potential contamination.
Pregnant women should be advised to seek medical advice if they experience fever or influenza-like symptoms, or if they are concerned that they could have acquired infection from a farm environment. Summary information about the four key infection hazards are given in the guidance, together with a link to related, general HSE advice for farmers and livestock keepers who have a responsibility to minimise the risks to pregnant women, including members of their family, the public and professional staff visiting farms.
4.1 Reference
- PHE/Defra/DH/HSE (January). Pregnancy: advice on contact with animals that are giving birth.
5. PHE research and applied epidemiology conference programme published
Public Health England’s Research and Applied Epidemiology Scientific Conference 2017, focusing on the application of epidemiological and other scientific methods to protect and improve public health, will be held on Tuesday 22 and Wednesday 22 March in the Ramphal Building at the University of Warwick.
The purpose of the annual event is to support high quality and innovative science through the sharing of good practice including the work of the NIHR Health Protection Research Units. The conference comprises a mix of plenary sessions, posters and parallel sessions.
Main session themes of the 2017 event include:
- healthcare associated infections
- innovative use of methodology and tools
- sexually transmissible infections and HIV
- use of modelling to inform vaccination policy
- improving outcomes for people who inject drugs
- application of whole genome sequencing to strengthen surveillance
- application of epidemiological methods to reduce health inequalities
- use of scientific methods to reduce the burden of chronic diseases
- using surveillance and routine data to inform public health action/response.
Further information: www.phe-events.org.uk/raesc17.
6. BSMT annual scientific meeting, PHE Colindale, 12 May
The British Society for Microbial Technology annual scientific meeting 2017 will be held at PHE Colindale on Friday 12 May. The programme includes the following presentations:
- Moving towards delivering precision medicine in sepsis: Professor Paul Dark (chair of critical care medicine, University of Manchester
- Cultivating the uncultured: Professor William Wade (professor of oral microbiology, Queen Mary University of London)
- Community-acquired pneumonia update: Dr Kate Templeton (consultant clinical scientist and honorary lecturer in medical microbiology, Royal Infirmary Edinburgh)
- Maldi-TOF mass spectrometry update – new applications (mycobacteria and fungi): Dr Belén Rodriguez Sanchez (Madrid Miguel Servet Fellow, Instituto de Investigación Sanitaria Gregorio Marañón)
- Multi-resistant Candida auris outbreaks: Dr Silke Schelenz (consultant microbiologist and infection control doctor, Royal Brompton Hospital)
- Laboratory detection of carbapenemase-producing enterobacteriaceae: Dr Katie Hopkins (PHE)
- Carbapenemase-resistant enterobacteriaceae - how de we cope with them clinically? Dr Kathy Bamford (Imperial College, London).
Further information: BSMT website.
